Are You Considering Stem Cell Treatment for Muscular Dystrophy?
Muscular dystrophies are inherited muscle disorders that have limited curative treatment options, with most only focusing on delaying disease progression and preventing further muscle damage or risk of respiratory infections in order to ensure a better quality-of-life for such individuals. Stem Cell Treatment however offers hope, with studies showing stem cell therapy can improve different muscular functions which are impaired in different forms of muscular dystrophies.
Read on to see if Muscular Dystrophy Stem Cell Treatment might be right for you.
Beike Biotechnology Muscular Dystrophy Patient Outcome Data
The table below presents the findings from a questionnaire completed by 43 patients who underwent stem cell treatment with Beike Cell Therapy for Muscular Dystrophy. This survey aimed to capture insights regarding patient satisfaction, the perceived effectiveness of the stem cell treatment, and any potential areas of enhancement.
The collected responses have been systematically arranged to offer a thorough overview of the patients’ experiences and outcomes.
How Stem Cell Therapy Improves Symptoms of Muscular Dystrophy
Stem cells are cells that are “pluripotent”, meaning they can differentiate into all other cells due to their self-renewing abilities. They can develop into ectodermal (ex. skin and some neurological structures), mesodermal (ex. bones, cartilages, and blood cells), or endodermal cells (ex. cells of internal body organs).
Therefore, injecting stem cells – from a donor – should theoretically allow them to differentiate and “replace” the damaged muscle fiber cells in different muscular dystrophies (5). Stem cell therapy has provided a new hope in curing or at least improving the symptoms associated with muscular dystrophies, in order to provide patients a better quality of life.
Following the testing of stem cell treatment on people with muscular dystrophy, in addition to their self-renewing abilities, stem cells have proven to have additional benefits other than tissue replacement; including (6):
- Replacing and repairing the damaged muscle fibers: As mentioned, this is their original function; to replace the damaged tissue – i.e. damaged muscle fibers in muscular dystrophies – through differentiating into these cells.
- Modulating the immune system and the ongoing inflammatory process: Stem cells produce different antioxidants; thereby reducing the muscle-destructive and atrophic process characterizing different muscular dystrophies.
- Inhibiting the rate of fibrosis: Studies have proven that in case of muscular dystrophy, stem cells prevent the deposition of fibrous tissues within the muscles; therefore decreasing scar formation and the degree of muscular dystrophy. This function is reported to be due to the immune modulation capacity of stem cells – as previously mentioned.
- Promoting vascular supply to the muscles: by stimulating the generation of new blood vessels (neovascularization/angiogenesis) through stimulating different vascular stimulating growth factors (ex. VEGF). Better blood supply allows for better and faster muscle repair and regeneration.
- Preventing cell death: Through releasing substances that can inhibit the process of apoptosis, or programmed cell death, of the damaged cells until they are adequately repaired by stem cells.
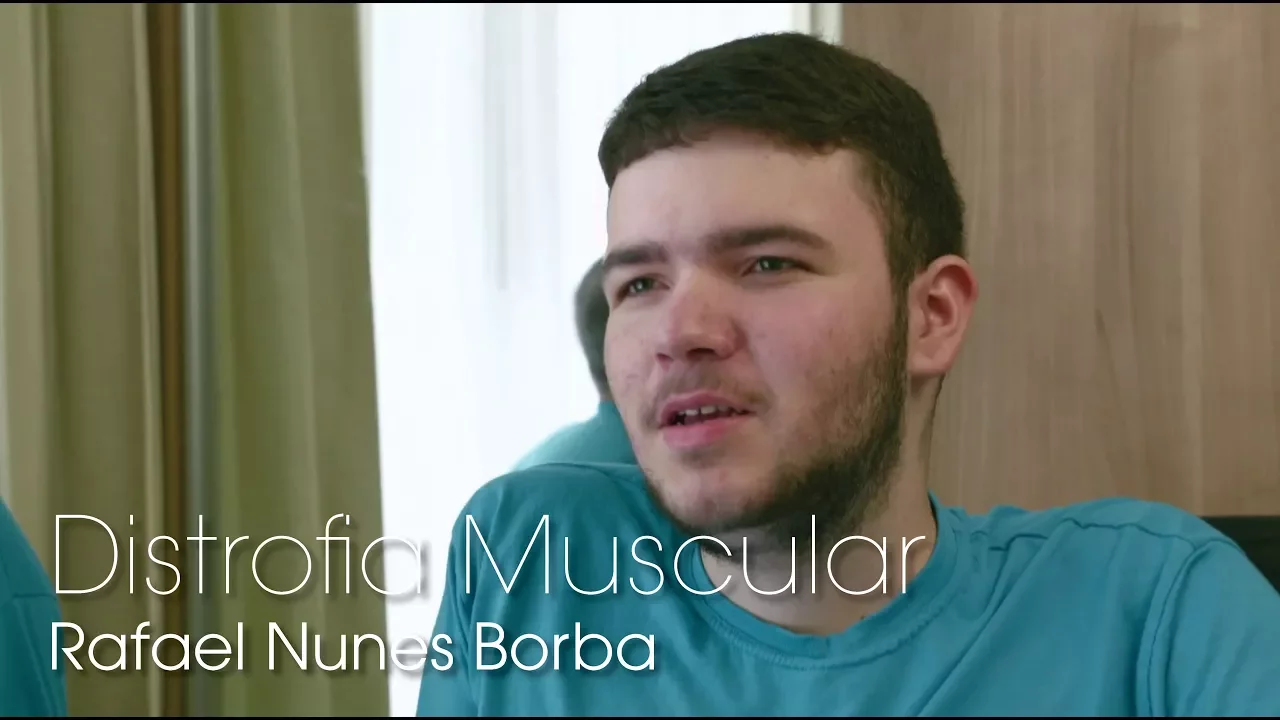
Rafael was diagnosed with muscular dystrophy as a child. Through stem cell treatment, he has seen a slowed disease progression. In this video he is undergoing his third comprehensive stem cell treatment procedure at our partner treatment hospital. His daily routines such as holding a glass, eating by himself, kicking a ball, typing on his phone or computer have gotten easier, leading to a better quality of life.
How can stem cells help relieve the symptoms of the muscular dystrophy for the patient?
Umbilical cord derived stem cells have been researched as novel option to treat muscular dystrophy in recent years. Most MD patients Beike has treated utilizing stem cells and rehabilitation showed visible signs of improvement. However, when discussing improvements, it is important to remember that they might greatly differ from one patient to another. This is due to many factors, such as the patient’s medical condition, severity of the disease, complications, general physical condition or age.
The purpose of stem cell treatment for Muscular Dystrophy is to promote the healing and growth of the affected muscles. Thus, various kinds of improvement are possible after our treatment and our past patients have experienced the following*:
- Enlarged muscle mass
- Increased muscle strength
- Decreased occurence of respiratory infection
- Improved balance
- Decreased stiffness
- Clinical stabilization
- Improved range of movement
- Decreased tremor occurrence
- Improved development (in children)
*It is important to remember that as for any medical treatment, improvements cannot be guaranteed. Please contact us for more information regarding the possible improvements for a particular case.
Our Treatment Program in Details
Beike is unlike any other stem cell treatment provider in the world, the reason? Since 2005, we have been developing and optimizing our stem cell treatment protocols with the concept that only a very comprehensive solution can allow our patients to truly benefit from stem cells. We believe that stimulation through various therapies is necessary to enhance stem cell regenerative response, therefore our protocols include daily therapies to support the stem cells. Finally, we provide a wide variety and large quantities of stem cells in order to adapt to each patient specific condition and deliver maximized regenerative potential.
Our stem cell therapy for muscular dystrophy program consist in 4 to 8 simple and minimally invasive injections of umbilical cord derived stem cells. The stem cells are transplanted using two separate methods: by intravenous way using a standard IV drip system, and through intramuscular injection in the affected muscles. These two delivery methods allow for increased efficacy while ensuring safety and minimum inconvenience for the patient.
- 15 to 18 Days Stay
- IV & intramuscular Injections
- UCBSC / UCMSC Cells
- Daily Therapy Program
- 120-400 Million Cells
- Nutrition Program
Patient Experience Stories
Find out more about patients previously treated with Beike stem cell protocols. The families participating in these blog posts talk about their stories and present their own view of the treatment, including thoughts regarding the daily therapies, the stem cell injection themselves as well as improvement noticed during and after treatment.
Stem Cell Quality and Quantity Ensured

Different types of stem cells for different needs
Beike provides stem cells from two separate sources: umbilical cord blood and umbilical cord tissue. Umbilical cord related samples are donated by healthy mothers after normal births and are sent to Beike Biotech’s laboratories for processing.
After reviewing the patient’s full medical information, our doctors will recommend which source of stem cells should be used for treatment. Our treatment protocols may include one or multiple types of stem cells in combination depending on each patient’s specific condition.
Highest International Stem Cell Processing Standards
Beike Biotechnology is processing its own adult stem cells in its internationally accredited laboratories. The company has full control over the processing and quality control of all stem cell products, ensuring perfect safety and highest quality.

Patient Videos
Below are video interviews recorded during treatment with Beike stem cells. The families showcased in these videos talk about their personal stories and their experience of the treatment including the improvement noticed.
The improvements mentioned in these videos are typical, however it does not guarantee that all patients may have the same improvements.
Why Choose Beike for a Stem Cell Treatment?
Experience: With more than a decade of practice, you are ensured to be advised and treated by competent professionals.
Safety: Backed by accreditations from national and international authorities we are dedicated to delivering the highest quality stem cells possible for your benefit.
Diversity: Multiple types of stem cells having different capabilities are available to adapt to each patient’s specific condition. We do not use the same type of stem cells for all patients.
Extensiveness: A complete supportive therapy program is provided daily to stimulate patient’s freshly transplanted stem cells. The best improvement can only be obtain by supporting your stem cells.
Support: A full follow-up program is provided after the treatment and you will be asked to take part in it at 1, 3, 6 and 12 months after treatment. Access to our team after the treatment is very important as you may receive further advice to maximize improvements.

Founded in July 2005, Shenzhen Beike Biotechnology is a national high-tech enterprise specialized in clinical transformation and technical service of biological treatment technology of strategic emerging industries.
Get more information now
Muscular Dystrophy Stem Cell Therapy FAQs
- What is Muscular Dystrophy?
Muscular dystrophies are a wide group of inherited disorders characterized by gradual weakness and wasting, or atrophy, of different body muscles. There are many types of muscle dystrophy, yet the most widely known type – and unfortunately the most severe – is Duchenne muscular dystrophy (DMD).
- Symptoms of Muscular Dystrophy
Symptoms of muscular dystrophy vary greatly depending on the type of defect – and therefore type of Muscular Dystrophy. For example, symptoms seen with DMD are more severe and rapidly progressing than those seen in milder forms such as Becker muscular dystrophy. The most common type of muscular dystrophy is DMD and it typically presents at around 4-5 years with (1, 2):
- Gradual muscle weakness and wasting
- Delay of reaching motor milestones
- Loss of previous ambulation (ex. Standing/walking)
- Recurrent respiratory complications (due to abnormal breathing muscles)
- Cardiac abnormalities (usually by the age of 20)
People with the more severe DMD form typically become wheelchair-ridden by the age of 12, and usually develop severe complications due to cardiac and respiratory complications – rather than due to direct muscular problems (1).
- Current Treatments for Muscular Dystrophy
Given that muscular dystrophies occur due to inherited genetic defects in the genes responsible for proper muscle development and functioning, its treatment options are limited, similar to lots of other inherited disorders. Current treatment options for muscular dystrophies include:
- Physiotherapy: Physiotherapy is still the main form of therapy for muscular dystrophy – along with steroids (2).
- Steroids: Steroids are strong anti-inflammatory drugs that can also modulate the body’s immune response. There is current evidence that early use of glucocorticoids/steroids delays the onset of wheelchair dependence. However, to this day and despite extensive studies on the topic, there are still uncertainties regarding which steroid is the best to use and the possible risk of under or over-treatment. This is also in addition to the potential side effects of prolonged steroid use such as weight gain and higher risk of infections (2).
- Gene Therapy: this is yet again another promising mode of therapy – similar to stem cell therapy – with multiple drugs being approved by the FDA for muscular dystrophies due to the limited amount of options available. These drugs target the gene abnormality responsible for muscular destruction and dystrophy; however given that these medications target a certain genetic mutation, they depend on a certain genetic mutation/aberration being present in the patient in order to be able to use it. For example, one drug approved known as Eteplirsen has been reported to be efficacious only in around 15% of patients with DMD who carry a certain mutation in Exon 15 of the DMD gene. This means that in children who have a gene abnormality elsewhere or even a different abnormality within the same gene – which is common – don’t benefit from this medication. Therefore, gene therapy requires a meticulous genetic assessment before its use (3, 4).
- Which Stem Cells are the Best to treat Muscular Dystrophy?
To date, there has not been a single study – to our knowledge – that has compared different types of stem cells, concerning safety and efficacy, particularly in patients with muscular dystrophies. However, we can summarize different stem cell sources that have been tested in these disorders. Each form of stem cells has its own benefits and drawbacks as will be mentioned. Different stem cell sources that have been tested in different muscle dystrophies – either on animals or in humans – include (5, 10):
- Mesenchymal Stem Cells: These are stem cells obtained from adipose tissues, bone marrow, or umbilical cord tissues – which we actually use at Beike. These cells are the most widely used stem cells since they can be easily produced in larger numbers to accommodate a higher number of patients and allow better efficacy, have a better response in neurological and muscular diseases, have better differentiation capacity into numerous cell types, and have better anti-cell death effect in case of degenerative conditions like muscular dystrophies that cause progressive muscle wasting – compared to other stem cells. Mesenchymal stem cells can be obtained from different sources including the umbilical cord, bone marrow, and adipose tissue.
- Muscle/Satellite Stem Cells: These are another type that has particular benefits in differentiating into the defective muscle fiber cells, of the same origin; though their use is limited in patients due to their limited migration abilities to the site of defect following their transplantation. These stem cells also require long-term suppression of immunity using immunosuppressants to prevent transplant rejection.
- Adult Pluripotent Stem Cells: These are another source that can be produced in large numbers, yet their differentiation abilities are limited.
- Embryonic Stem Cells: Another type of stem cell includes embryonic stem cells. These cells can also differentiate into photoreceptors, yet they are difficult to obtain and have ethical concerns regarding their sources.
After carefully reviewing all of the benefits and risks of each type, we have decided to use mesenchymal umbilical cord-based stem cells as our main source since they have been the most extensively studied type in neuromuscular conditions, including muscular dystrophy, with the least reported side effects (6). This is in addition to also using umbilical cord blood cells (hematopoietic cells) concurrently to provide additional benefits from using two types of stem cells; with each contributing to muscle and nerve regeneration through different complementary mechanisms.
In addition to the source of stem cells, there are also multiple routes of stem cell administration. Most clinical trials testing stem cell therapy in Muscular Dystrophy use either one – or both – of preferably two routes; which are (10):
- Intravenous (Into the blood)
- Intramuscular (Locally into the muscles)
Studies have shown that in contrast to a single route of intravenous administration, administering stem cells through dual administration provides significant clinical results and improvement (10). At Beike, we use combined intravenous and intramuscular routes concomitantly to achieve the best results with the least possible side effects.
- Which Stem Cells Do We Use for Treating Muscular Dystrophy?
At Beike, we use umbilical cord stem cells for muscle dystrophies, both umbilical cord-related mesenchymal/tissue and blood/hematopoietic cell samples donated from healthy mothers after a normal birth. As previously mentioned, this concomitant administration of both types of stem cells, mesenchymal and hematopoietic stem cells, provides better results.
- Optimum Timing for Stem Cell Therapy for Muscular Dystrophy
There is no specific timing for stem cell treatment, but like many other neurological conditions, we generally recommend seeking stem cell therapy early after diagnosis – i.e. during childhood. This is because the earlier the stem cell intervention, the easier it is to prevent further damage to the muscle fibers and to be able to restore normal mobile functioning before permanent damage and muscle atrophy/wasting take place.
We still need to report that clinical benefit is not 100% guaranteed as is the case with any intervention, and consulting our specialists prior to undergoing the procedure is of utmost importance in order to gain more insight into the procedure and the estimated possibility of treatment success for your individual case.
- Possible Side Effects of Stem Cell Therapy for Muscular Dystrophy
Of course, no treatment is without complications, and stem cell therapy is the same. However, despite its novelty, mesenchymal stem cell therapy has limited side effects, if used properly, with comparable general side effects to those experienced with regular blood transfusion or foreign organ transplantation (ex. allergic reactions, cell rejection, or fever). Additionally, in studies specifically studying stem cell therapy in patients with Muscular Dystrophy, no significant side effects were reported and none were life-threatening or had life-long consequences when mesenchymal stem cells were used (10). They were also easily managed medically at the time of their occurrence.
References
1. Falzarano MS, Scotton C, Passarelli C, Ferlini A. Duchenne Muscular Dystrophy: From Diagnosis to Therapy. Molecules (Basel, Switzerland). 2015;20(10):18168-84. Available from: https://www.mdpi.com/1420-3049/20/10/18168
2. Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Brumbaugh D, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. The Lancet Neurology. 2018;17(3):251-67. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5869704/
3. Elangkovan N, Dickson G. Gene Therapy for Duchenne Muscular Dystrophy. Journal of neuromuscular diseases. 2021;8(s2):S303-s16. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8673537/
4. Lim KR, Maruyama R, Yokota T. Eteplirsen in the treatment of Duchenne muscular dystrophy. Drug design, development and therapy. 2017;11:533-45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5338848/
5. Sienkiewicz D, Kulak W, Okurowska-Zawada B, Paszko-Patej G, Kawnik K. Duchenne muscular dystrophy: current cell therapies. Therapeutic advances in neurological disorders. 2015;8(4):166-77. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4480531/
6. Abdelbakey AEO, Soliman WT, Abo Elkheir W, Ali AE. Stem cell therapy as a potential therapy for Duchenne muscular dystrophy. Minia Journal of Medical Research. 2020;31(3):13-7. Available from: https://mjmr.journals.ekb.eg/article_219852_cba4685af15a1359aecf97306dcfae1c.pdf
7. Sharma A, Sane H, Paranjape A, Bhagawanani K, Gokulchandran N, Badhe P. Autologous bone marrow mononuclear cell transplantation in Duchenne muscular dystrophy – a case report. The American journal of case reports. 2014;15:128-34. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3976215/
8. Dai A, Baspinar O, Yeşilyurt A, Sun E, Aydemir Ç, Öztel ON, et al. Efficacy of stem cell therapy in ambulatory and nonambulatory children with Duchenne muscular dystrophy – Phase I-II. Degenerative neurological and neuromuscular disease. 2018;8:63-77. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6207384/
9. Sharma A, Sane H, Badhe P, Gokulchandran N, Kulkarni P, Lohiya M, et al. A Clinical Study Shows Safety and Efficacy of Autologous Bone Marrow Mononuclear Cell Therapy to Improve Quality of Life in Muscular Dystrophy Patients. Cell Transplantation. 2013;22(1_suppl):127-38. Available from: https://pubmed.ncbi.nlm.nih.gov/24070109/
10. Biressi S, Filareto A, Rando TA. Stem cell therapy for muscular dystrophies. The Journal of clinical investigation. 2020;130(11):5652-64. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7598050/